Behavioral Health
Advancing Behavioral Health & Crisis Care
Initium has a proven track record in behavioral health. Our team brings decades of experience working at the intersection of behavioral health, health systems, and the community. We understand the numerous entities involved in this ecosystem and have successfully coordinated efforts across stakeholders to address the unmet behavioral health needs of communities. Our experience working with both rural and urban communities and our healthcare acumen have helped us develop an innovative approach to building comprehensive behavioral health strategies based on national best practices.
The Crisis Continuum
Initium Health is fluent in the research that shows that implementing the Crisis Continuum is the most effective option, while also being the least restrictive and the least costly.

Implementing the Crisis Continuum in a community means the decreased use of jails, emergency departments, and inpatient settings by intervening in earlier stages of crisis, and it means that people get the help they need. Since its launch in July 2022, the national 988 Suicide and Crisis Lifeline has answered over 10 million calls from people experiencing a mental health or substance use crisis, addressing the Someone to Call aspect of the Crisis Continuum.
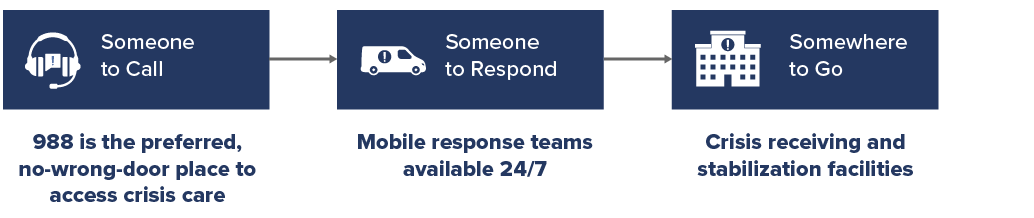
For 20% of callers, a phone call may not be enough. Mobile crisis teams may need to be dispatched as Someone to Respond, teams who are trained in behavioral health crises. If the crisis cannot be resolved in the field, they may need Somewhere to Go, a crisis stabilization facility that can help stabilize the person and link them into care and follow-up. Initium Health works with communities to identify gaps in their crisis services and collaboratively work toward solutions to fill those gaps, including with the creation of new crisis stabilization facilities.
Behavioral Health Integration
National best practices indicate that the most effective ways to rapidly address these crises are:
- Having and promoting a robust crisis continuum and
- Behavioral Health Integration (BHI) into primary medical care
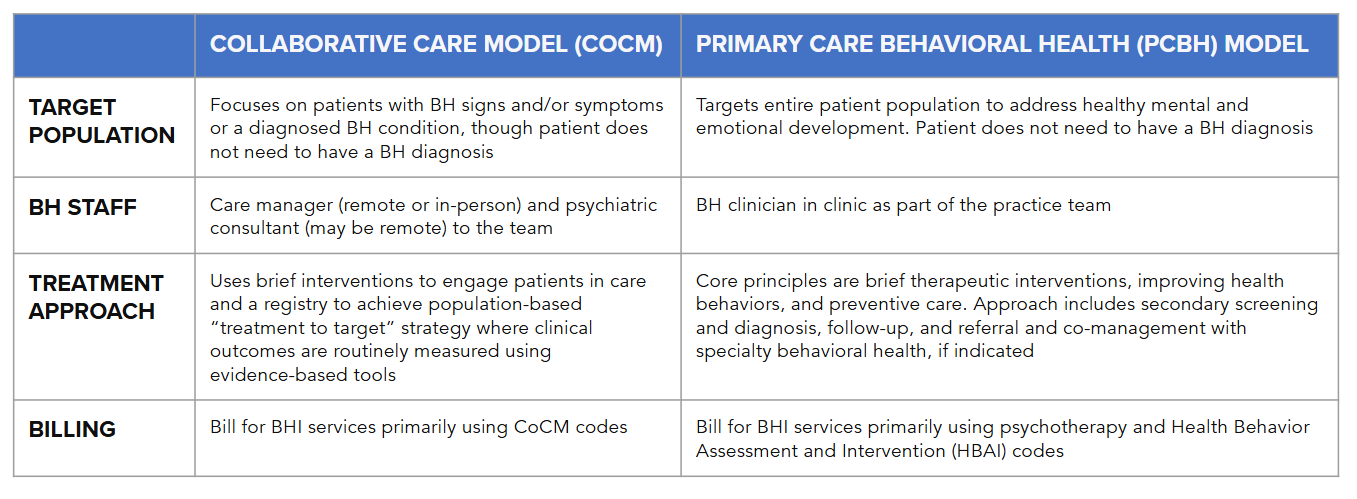
The research is clear that patients benefit when physical health and behavioral health are treated concurrently. Whether the medical team is primary care or a specialty practice, almost every major medical organization currently recommends integration of the physical health team and the behavioral health (mental health and substance use disorders) teams, rather than keeping them entirely separate.
Because different models work better for different practices, and because the funding streams for reimbursement are varied, Initium Health consults with practices to aid them on their journey to Behavioral Health Integration (BHI).
We stay abreast of changes to reimbursement that can make your BHI transition more gratifying for patients and providers, and more profitable for your organization’s bottom line.
Feasibility Studies
We support government agencies and health systems to analyze existing behavioral health services, identify gaps, and develop cost-effective and comprehensive solutions. Our team brings together physicians, public health professionals, healthcare executives, and construction experts, along with a cadre of expert project managers, researchers, and financial analysts. Our feasibility studies address clinical, operational, and financial needs along with site and facility requirements and design recommendations.
Behavioral Health Gap Analysis
Assess population needs and gaps in services currently available
Service Needs and Projections
Define services and projected utilization, current and future
Financial Analysis
Capital and operational costs, reimbursement, and funding opportunities
Solution Design
Facility and programmatic design to meet community needs
Benefit Analysis
Projected benefits to community from new services
Community Engagement
Our community engagement process intentionally addresses the unique needs of diverse populations, including people experiencing homelessness, people with disabilities, and people of color. We built trust with each stakeholder and community by valuing their input, through active participation, and by encouraging belief in a shared vision. This allows us to ensure that the services developed by our clients will be accessed by those who need them most. We partner with our clients and their communities to raise awareness, break down silos, and unite stakeholders to inspire meaningful change.

Community listening sessions and charrettes

1-1 and small group interviews
Social media outreach and engagements
Hyper-local influencer campaigns

On-the-ground meetings and organic connections
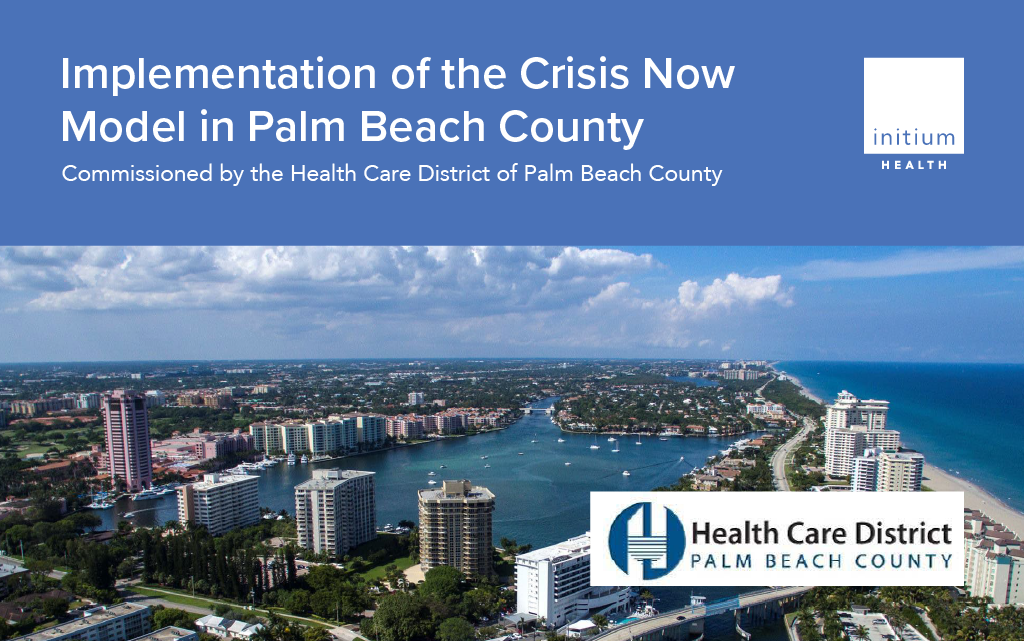
Health Care District of Palm Beach County
This report details the current state of crisis care in Palm Beach County, evaluates the current state in light of the National Guidelines for Behavioral Health Crisis Care and provides recommendations to address these factors and increase the availability of high-quality crisis care throughout the county.
Eastern New Mexico

Crisis Continuum of Care
We provide a comprehensive evaluation of crisis care for mental health and substance use disorders. We map the patient journey, identify resource gaps, and develop solutions that reflect national guidelines and leading-edge practices, so communities can confidently invest resources in what works.

Public Awareness Campaigns
By using a holistic, public health-based approach, our team creates innovate campaigns that educate both general and at-risk populations about behavioral health resources available to help during a time of crisis, such as the 988 Suicide & Crisis Lifeline.

Behavioral Health Footprint Expansion
We developed an innovative partnership where federal funding, private partners and a health system established a sustainable model of supportive behavioral health which increased access, reduced the system heath spend on frequent utilizers of the emergency room and addressed a great community need.

Integrated Care
We leveraged state, federal and philanthropic funding along with emerging technology to develop a robust system of care which reduced cost, improved patient and provider satisfaction, and developed a sustainable infrastructure for an integrated health system.
OUR CLIENTS

OneFifteen
A Non-profit recovery ecosystem dedicated to helping people live free of addiction
The organization believes successful recovery is achieved through personalized, evidence-based care and unwavering support from care providers and the community.
OneFifteen’s flagship program is based in Dayton, Ohio, a campus that provides a full continuum of services, including outpatient and inpatient treatment, crisis stabilization and rehabilitation housing, as well as wraparound services such as vocational training.

Model: Recovery Housing Outpatient and Inpatient Treatment
Location: Dayton, OH

”It doesn’t matter where you come from, our doors are open.”



The McAuley Residence
Housing for Recovering Women and their Children
The McAuley Residence, currently located on State Street in Portland, serves women who struggle with addiction and have experienced other problems such as homelessness, domestic violence, broken relationships, mental health issues, or incarceration. The Residence gives women access to health and dental services and life skills programs.
“Women enter in a state of homelessness, hopelessness, and then they transition, over a period of time, into very powerful women, ready to take on any aspect of life’s inevitable challenges.”
— Mercy Hospital
Location: Portland, ME